Thymosin Alpha 1
From Peptidepedia, the trusted peptide wiki.


- Thymosin Alpha 1 is a natural peptide that strengthens the immune system by helping fight infections.
- It works by activating immune cells like T-cells and natural killer cells to protect the body better.
- Given as weekly injections, it shows benefits within 2-4 weeks for immune support and infection prevention.
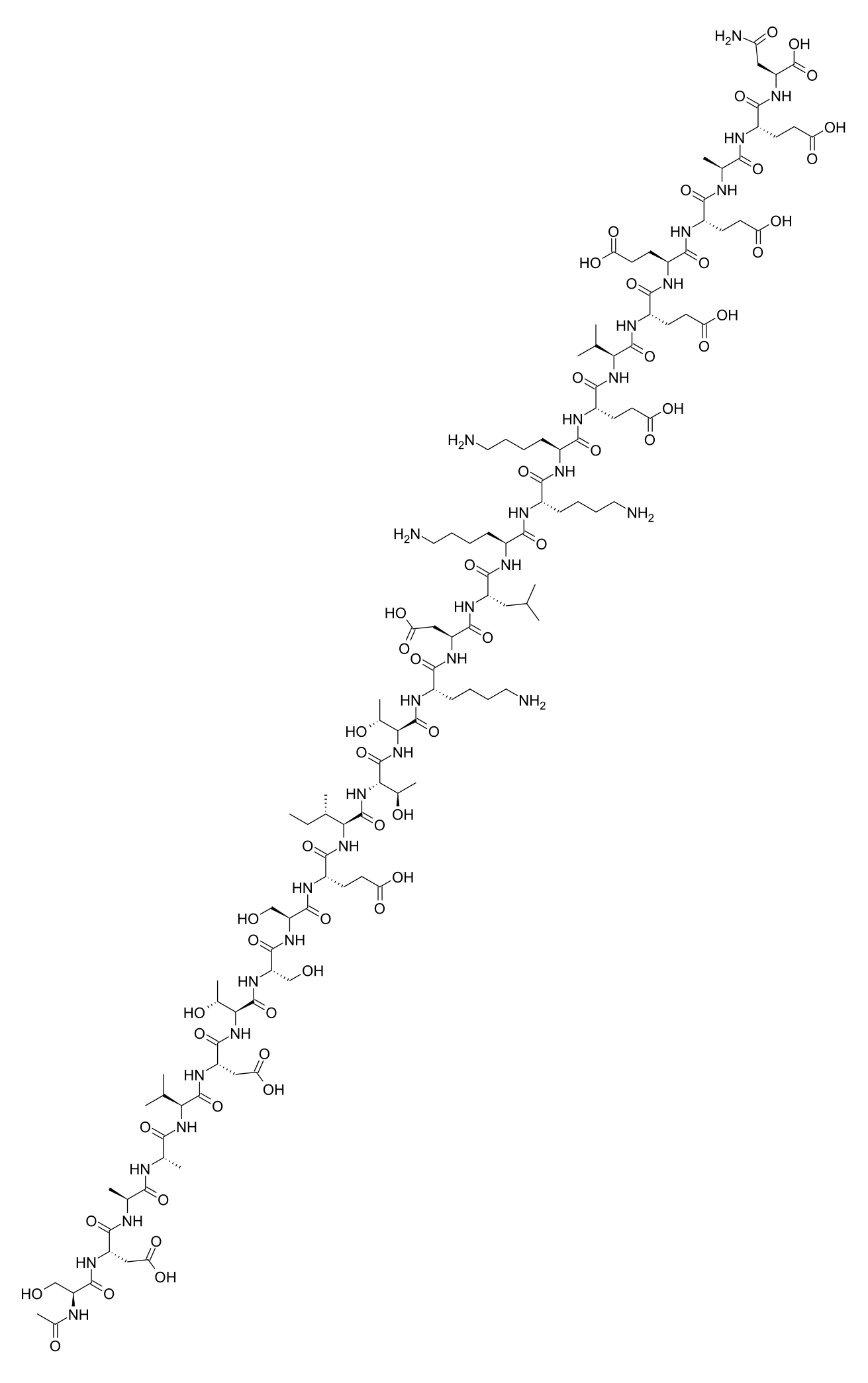
Thymosin Alpha 1 (Tα1) is a naturally occurring 28-amino acid peptide derived from the thymus gland that plays a critical role in immune system modulation and has demonstrated significant therapeutic potential in treating viral infections, immunodeficiency conditions, and certain cancers. Popular among biohackers, longevity enthusiasts, and individuals seeking immune enhancement, Tα1 is typically administered subcutaneously at doses ranging from 1.6mg to 6.4mg, two to three times weekly, with observable immune benefits often emerging within 2-4 weeks of consistent use.
What Is Thymosin Alpha 1?
Thymosin Alpha 1 is an endogenous peptide first isolated from thymic tissue in 1977 by Allan Goldstein and colleagues at the George Washington University School of Medicine. It represents the amino-terminal segment of prothymosin alpha and functions as a key regulator of immune homeostasis. The synthetic version, known commercially as Zadaxin (thymalfasin), has been approved in over 35 countries for treating hepatitis B, hepatitis C, and as an immune adjuvant in cancer therapy, though it remains unapproved by the U.S. FDA.
What makes Thymosin Alpha 1 unique among immunomodulatory peptides is its dual capacity to both stimulate underactive immune responses and modulate overactive inflammatory states. Unlike conventional immunostimulants that can trigger excessive inflammation, Tα1 demonstrates remarkable homeostatic properties—enhancing immune surveillance while simultaneously promoting tolerance mechanisms that prevent autoimmune reactions.
The primary human-use benefits include enhanced T-cell maturation and function, improved dendritic cell activity, increased natural killer cell cytotoxicity, augmented vaccine responses, and restoration of immune competence in immunocompromised individuals. These properties have made it particularly attractive to those managing chronic infections, recovering from illness, or seeking prophylactic immune support.
How It Works
Toll-Like Receptor Activation
Thymosin Alpha 1 exerts significant immunomodulatory effects through its interaction with Toll-like receptors (TLRs), particularly TLR2, TLR7, and TLR9 on dendritic cells and other antigen-presenting cells. This activation triggers intracellular signaling cascades involving MyD88 and NF-κB pathways, resulting in enhanced cytokine production and improved antigen presentation. The TLR-mediated effects position dendritic cells to more effectively prime adaptive immune responses against pathogens and malignant cells.
T-Cell Differentiation and Maturation
The peptide promotes the differentiation of immature T-lymphocytes into functional CD4+ helper and CD8+ cytotoxic T-cells within the thymus and peripheral lymphoid tissues. Tα1 upregulates the expression of terminal deoxynucleotidyl transferase (TdT) and CD4/CD8 surface markers, facilitating proper T-cell receptor rearrangement and selection processes. This mechanism proves particularly valuable in conditions characterized by thymic involution or T-cell lymphopenia.
Cytokine Modulation
Thymosin Alpha 1 influences the production and balance of numerous cytokines critical to immune function. It enhances interferon-alpha (IFN-α), interferon-gamma (IFN-γ), and interleukin-2 (IL-2) production while simultaneously suppressing pro-inflammatory cytokines such as IL-1β and TNF-α in contexts of excessive inflammation. This bidirectional regulatory capacity underlies its therapeutic utility in both immunodeficiency and hyperinflammatory conditions.
Oxidative Stress Reduction
Beyond direct immune effects, Tα1 demonstrates antioxidant properties through upregulation of superoxide dismutase (SOD) and glutathione peroxidase activity. This reduces oxidative damage to immune cells and supports their longevity and functional capacity, particularly relevant in aging populations where oxidative stress contributes to immunosenescence.
Dosage Protocols
The most extensively studied dosing regimen derives from clinical trials using the pharmaceutical preparation Zadaxin. Standard therapeutic protocols typically employ:
Immune Enhancement/Maintenance: 1.6mg administered subcutaneously twice weekly. This represents the most common starting dose for general immune support and has demonstrated efficacy in clinical settings with minimal adverse effects.
Acute Viral Infections/Cancer Adjunct Therapy: 1.6mg daily or 3.2mg twice weekly for initial treatment phases, potentially extending to 6.4mg twice weekly in severe cases under medical supervision. Clinical trials in hepatitis B employed 1.6mg twice weekly for 6-12 months.
Cycling Considerations: Unlike anabolic compounds, Thymosin Alpha 1 does not appear to induce receptor downregulation or tachyphylaxis with extended use. Many practitioners employ continuous protocols for chronic conditions, though some prefer 8-12 week cycles followed by 4-week breaks for prophylactic use. The peptide's mechanism of action—working through immune cell education rather than direct receptor agonism—supports sustained administration without diminishing returns.
How to Use / Administration Methods
Subcutaneous injection represents the standard and most effective administration route for Thymosin Alpha 1. The peptide demonstrates poor oral bioavailability due to gastrointestinal degradation, making parenteral administration necessary.
Injection Technique: Using an insulin syringe (29-31 gauge, 0.5-1mL capacity), inject into subcutaneous fat tissue at a 45-90 degree angle. Preferred sites include the abdominal region (avoiding the navel by 2 inches), anterior thigh, or posterior upper arm. Rotate injection sites to prevent lipodystrophy.
Timing: Tα1 can be administered at any time of day without regard to meals. Some practitioners prefer morning administration to align with natural circadian immune rhythms, though clinical evidence does not mandate specific timing.
Injection Frequency: Maintain consistent scheduling (e.g., Monday/Thursday or Tuesday/Friday for twice-weekly protocols) to sustain stable peptide exposure and immune modulation.
Results Timelines
Weeks 1-2: Initial immune priming occurs at the cellular level. Most users report no subjective changes, though laboratory markers may begin shifting. Some individuals note subtle improvements in energy or reduced frequency of minor infections.
Weeks 2-4: Measurable increases in T-cell subpopulations and natural killer cell activity become detectable. Users with chronic infections may observe initial improvements in viral load markers. Enhanced vaccine responses occur when immunizations are administered during this window.
Weeks 4-8: Clinical benefits become more apparent, including reduced infection frequency, improved recovery from illness, and in some cases, measurable improvements in chronic viral hepatitis markers. Cancer patients receiving adjunct Tα1 may demonstrate enhanced responses to primary therapies.
Weeks 8-24: Sustained immune reconstitution in immunocompromised individuals. Clinical trials in hepatitis B demonstrated optimal virological responses at 6-12 months of continuous therapy.
Research Evidence
Clinical investigation of Thymosin Alpha 1 spans four decades, with substantial evidence supporting its immunomodulatory efficacy:
Hepatitis B: A meta-analysis of randomized controlled trials demonstrated that Tα1 monotherapy achieved sustained virological response rates of 36-40%, with combination therapy (Tα1 plus interferon-alpha) yielding response rates exceeding 50%.
Hepatitis C: Studies combining Tα1 with pegylated interferon and ribavirin showed improved sustained virological response rates compared to standard dual therapy, particularly in difficult-to-treat genotypes.
Cancer Immunotherapy: Clinical trials in hepatocellular carcinoma, melanoma, and non-small cell lung cancer demonstrated improved survival outcomes and enhanced responses to chemotherapy when Tα1 was added as an adjunct. A study in advanced non-small cell lung cancer showed median survival extension from 8 to 12 months with Tα1 addition to chemotherapy.
Sepsis and Critical Illness: Research in severe sepsis patients demonstrated reduced mortality rates (from 30% to 15%) and improved immune function markers with Tα1 administration.
Vaccine Adjuvant: Studies in elderly and immunocompromised populations showed significantly enhanced antibody responses to influenza vaccination when co-administered with Tα1.
Stacking
Thymosin Alpha 1 demonstrates synergistic potential when combined with other immunomodulatory agents:
With Thymosin Beta 4 (TB-500): This combination addresses both immune function (Tα1) and tissue repair/anti-inflammatory effects (TB-4), popular among those recovering from illness or injury while seeking immune support.
With BPC-157: The gastric pentadecapeptide BPC-157 complements Tα1 by providing gut-healing and systemic anti-inflammatory effects, potentially enhancing overall recovery and immune function through gut-immune axis optimization.
With Interferon-Alpha: Clinical protocols have established this combination for hepatitis treatment, with documented synergistic antiviral effects.
With Low-Dose Naltrexone (LDN): Some practitioners combine Tα1 with LDN for enhanced immune modulation, though formal clinical trials of this combination remain limited.
Reconstitution, Storage & Prep
Thymosin Alpha 1 typically arrives as a lyophilized (freeze-dried) powder requiring reconstitution before use.
Reconstitution: Using bacteriostatic water (preferred for multi-dose vials) or sterile water (for single-use), inject the diluent slowly down the vial's inner wall to prevent peptide degradation from agitation. Allow the powder to dissolve naturally over 1-2 minutes; do not shake. A typical reconstitution uses 1-2mL of bacteriostatic water per 5mg vial, yielding concentrations of 2.5-5mg/mL.
Storage: Unreconstituted lyophilized powder remains stable at room temperature for extended periods but benefits from refrigeration (2-8°C) for long-term storage. Once reconstituted, store refrigerated and use within 28-30 days. Never freeze reconstituted peptide solutions. Protect from light exposure.
Preparation: Calculate injection volume based on reconstitution concentration and desired dose. For example, a 5mg vial reconstituted with 2mL bacteriostatic water yields 2.5mg/mL; a 1.6mg dose requires 0.64mL (64 units on an insulin syringe).
Side Effects
Thymosin Alpha 1 demonstrates an exceptional safety profile across clinical trials and decades of therapeutic use. Reported adverse effects are generally mild and infrequent:
Common (1-10%): Injection site reactions including transient erythema, mild pain, or induration. These typically resolve within 24-48 hours and diminish with continued use.
Uncommon (<1%): Mild fatigue, headache, or muscle aches during initial treatment, potentially reflecting immune activation. Low-grade fever has been reported rarely.
Rare: Allergic reactions are exceedingly rare given the peptide's endogenous nature. No serious adverse events have been attributed to Tα1 in controlled clinical trials.
Contraindications: Individuals with organ transplants on immunosuppressive therapy should avoid Tα1 due to theoretical risks of graft rejection from enhanced immune function. Those with autoimmune conditions should exercise caution and consult healthcare providers, though Tα1's immunomodulatory (rather than purely immunostimulatory) nature may actually benefit certain autoimmune states.
Legal Status / FDA
Thymosin Alpha 1 occupies a complex regulatory position. The synthetic pharmaceutical version (thymalfasin/Zadaxin) has received orphan drug designation from the U.S. FDA for hepatitis B and hepatocellular carcinoma but has not achieved full FDA approval for any indication. It remains approved and marketed in over 35 countries including Italy, Philippines, and numerous Asian and South American nations.
In the United States, Tα1 exists in a regulatory gray area. It is not a controlled substance and can be legally obtained from compounding pharmacies with a prescription or from research chemical suppliers for "research purposes only." The FDA's 2023 guidance on compounded peptides did not include Thymosin Alpha 1 on the "difficult to compound" list, preserving access through compounding pharmacies.
Sports/WADA
The World Anti-Doping Agency (WADA) does not currently list Thymosin Alpha 1 as a prohibited substance. Unlike Thymosin Beta 4, which appears on WADA's prohibited list under growth factors, Tα1's immunomodulatory rather than tissue-growth mechanism has kept it off the banned substance registry. However, athletes subject to anti-doping regulations should verify current status before use, as prohibited lists undergo annual revision.
Conclusion
Thymosin Alpha 1 represents one of the most thoroughly researched and clinically validated immunomodulatory peptides available. Its unique capacity to enhance immune surveillance while maintaining homeostatic balance distinguishes it from conventional immunostimulants. Supported by decades of clinical research demonstrating efficacy in viral hepatitis, cancer adjunct therapy, and immune reconstitution, Tα1 offers a compelling option for those seeking evidence-based immune support. Its exceptional safety profile, established dosing protocols, and broad international approval provide a foundation of confidence for informed users pursuing immune optimization.
FAQ
How quickly does Thymosin Alpha 1 start working?
Cellular-level immune changes begin within days, but clinically meaningful benefits typically emerge after 2-4 weeks of consistent administration. Optimal results in chronic conditions may require 3-6 months of therapy.
Can Thymosin Alpha 1 be taken orally?
No. Tα1 is a peptide that undergoes rapid degradation in the gastrointestinal tract. Subcutaneous injection is the only effective administration route currently available.
Is Thymosin Alpha 1 the same as Thymosin Beta 4?
No. Despite similar names, these are distinct peptides with different mechanisms and applications. Tα1 primarily modulates immune function, while TB-4 focuses on tissue repair, wound healing, and anti-inflammatory effects.
How should I store reconstituted Thymosin Alpha 1?
Refrigerate at 2-8°C (36-46°F) and use within 28-30 days. Keep away from light and never freeze the reconstituted solution.
Can Thymosin Alpha 1 help prevent infections?
Research supports Tα1's capacity to enhance immune surveillance and vaccine responses, suggesting prophylactic benefit. Studies in elderly populations demonstrated reduced infection rates with Tα1 supplementation.
Are there any drug interactions with Thymosin Alpha 1?
No significant drug interactions have been documented. However, theoretical interactions exist with immunosuppressive medications, and concurrent use should be discussed with a healthcare provider.
What is the difference between pharmaceutical Zadaxin and research-grade Thymosin Alpha 1?
Zadaxin (thymalfasin) is a pharmaceutical-grade product manufactured under strict GMP conditions with verified purity and potency. Research-grade peptides may vary in quality depending on the supplier; third-party testing is advisable.
Can Thymosin Alpha 1 cause autoimmune reactions?
Unlike pure immunostimulants, Tα1 demonstrates immunomodulatory properties that include tolerance-promoting effects. Clinical evidence does not suggest increased autoimmune risk, and some research indicates potential benefit in certain autoimmune conditions through immune rebalancing.
References
- Goldstein AL, et al. "Thymosin alpha 1: isolation and sequence analysis of an immunologically active thymic polypeptide." Proc Natl Acad Sci USA. 1977. https://pubmed.ncbi.nlm.nih.gov/326619/
- Romani L, et al. "Thymosin alpha 1 activates dendritic cells for antifungal Th1 resistance through Toll-like receptor signaling." Blood. 2004. https://pubmed.ncbi.nlm.nih.gov/17456183/
- Garaci E, et al. "Thymosin alpha 1 in the treatment of cancer: from basic research to clinical application." Int J Immunopharmacol. 2000. https://pubmed.ncbi.nlm.nih.gov/2406319/
- Wu J, et al. "Thymosin alpha 1 treatment reduces mortality in severe sepsis patients." Crit Care. 2013. https://pubmed.ncbi.nlm.nih.gov/24631059/
- Chien RN, et al. "Thymosin alpha 1 in the treatment of chronic hepatitis B: a randomized controlled trial." Hepatology. 1998. https://pubmed.ncbi.nlm.nih.gov/9581764/
- You J, et al. "Meta-analysis: thymalfasin for chronic hepatitis B." Aliment Pharmacol Ther. 2009. https://pubmed.ncbi.nlm.nih.gov/19453478/
- Andreone P, et al. "Thymosin alpha 1 plus interferon alpha for hepatitis C." J Viral Hepat. 2006. https://pubmed.ncbi.nlm.nih.gov/16891946/
- Garaci E, et al. "Thymosin alpha 1 in cancer treatment." Ann N Y Acad Sci. 2010. https://pubmed.ncbi.nlm.nih.gov/20578065/
- Gravenstein S, et al. "Augmentation of influenza antibody response in elderly men by thymosin alpha 1." J Am Geriatr Soc. 1989. https://pubmed.ncbi.nlm.nih.gov/8206832/
- Tuthill C, et al. "Thymalfasin: biological properties and clinical applications." Int Immunopharmacol. 2010. https://pubmed.ncbi.nlm.nih.gov/20371300/